Some days it feels as though there’s an invisible timer running between my hand and my brain. Then, whenever my rare disease decides that I’ve done too much – or it gets too cold or hot, or for no reason – the timer goes off in my hand and lower arm. The timer’s alarm isn’t a buzzer, though, it’s neuropathic pain. These pain flares are bad enough to literally drop me to my knees; I’ll either faint or vomit, from pain. Neither is a particularly good option, trust me!
As an example, last night I went out to dinner with friends. We had a wonderful time, and the hours just flew by; we chatted from 1800 right through to 2130, over excellent food. By the time I got home at about 2200 (that’s 10 PM for those of you not used to ‘military time’!), one of these CRPS pain flares was well underway.
Complex Regional Pain Syndrome is a truly nasty disease, both autoimmune and neuro-inflammatory. It generally affects the limbs, an arm or a leg; or some combination of these extremities. Although my CRPS was diagnosed only in my right hand and lower arm, back in 2016, the condition affects my entire life.
First there are the symptoms of autoimmune illness, which include; fatigue, severe joint pain, swelling, ankylosis-like adhesions that form within the joints of my fingers and wrist; it feels as though scar tissue is constantly growing between these joints. My physiotherapist breaks up these adhesions, using manipulation and mobilization therapy, on a regular basis. And yes, that process is very painful.
The neuro-inflammatory side of the condition is what causes my allodynia and neuropathic pain. Allodynia is a painful skin sensitivity to touch, to cold or warm temperatures, to fabrics (clothing), to humidity, even to airflow or a light breeze. Simply breathing on my hand can trigger my allodynia!
The neuropathic pain can a feeling that the skin of the affected area is constantly being rubbed with sandpaper, or being stung by insects. Sometimes it feels as though my hand and arm are receiving electric shocks, right along the nerve pathways.
Since late 2018, the neuro-inflammatory facet of CRPS has also been causing mild cognitive impairment or MCI. I’m thankful that it’s mild, but developing cognitive impairment in your early 50s really isn’t much fun. Because of this new symptom, I’ve had to step away from a career that I adored – in bioethics or biomedical ethics – and from my dream job.
In more scientific terms:
complex regional pain syndrome (CRPS) – multiple system dysfunction, severe and often chronic pain, and disability – can be triggered by a minor injury, a fact that has fascinated scientists and perplexed clinicians for decades…
Compelling evidence implicates biological pathways that underlie aberrant inflammation, vasomotor dysfunction, and maladaptive neuroplasticity in the clinical features of CRPS.
Collectively, the evidence points to CRPS being a multifactorial disorder”.(1)
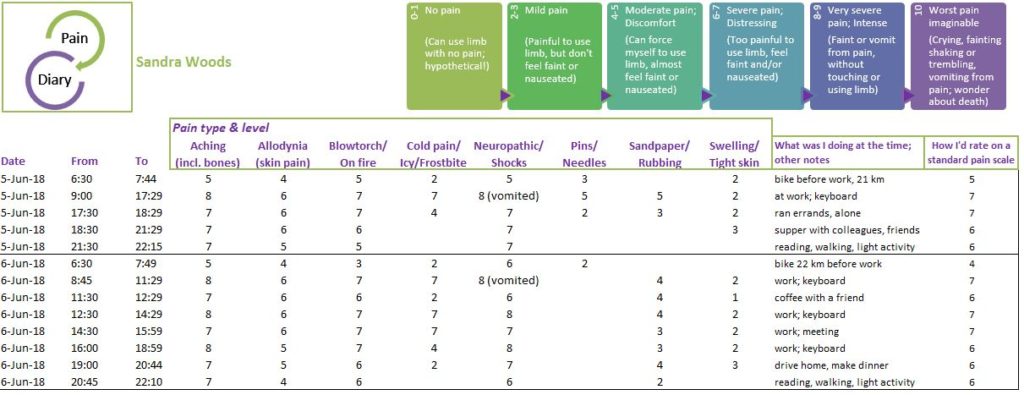
In plain English, at any given moment I’ll be experiencing a certain degree of full-body fatigue along with about seven different types of pain – all with varying degrees of severity. As I write this, it’s the cold neuropathic pain which is in the lead, the one that feels the most severe. About a 7 out of 10 on my own pain scale; “Severe pain; Distressing (Too painful to use limb, feel faint and/or nauseated)”.
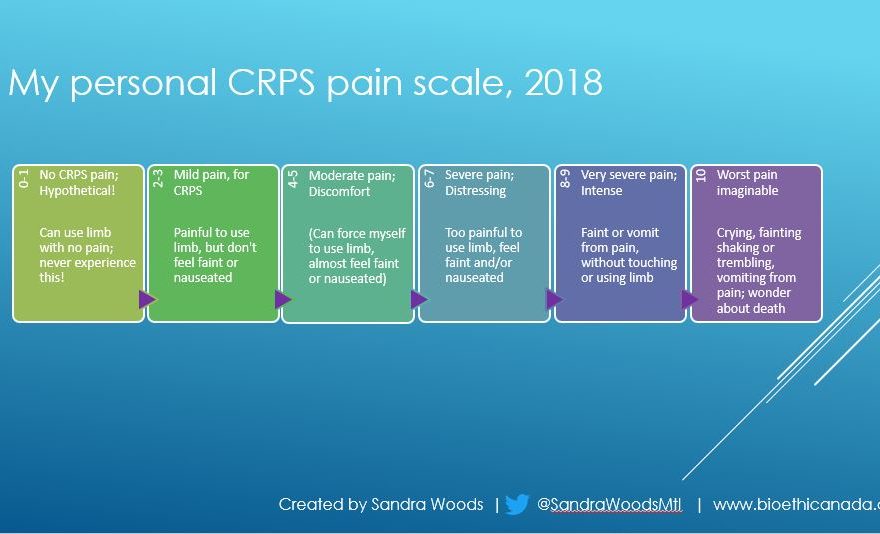
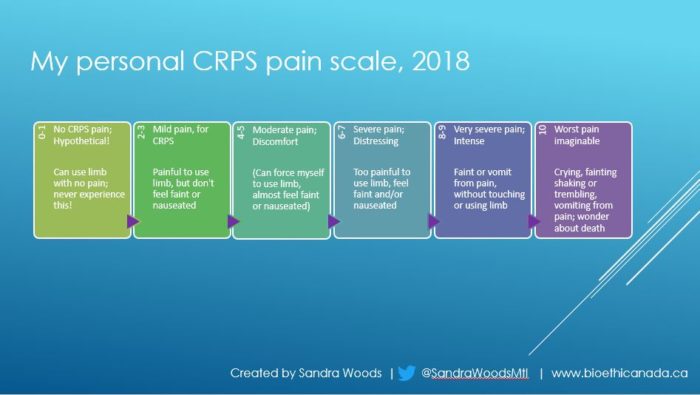
Back in 2018, I got so frustrated with the pain scales that I had been asked to complete after a full-body infusion of anesthetic medication, that I created my own!
Of course, one inherent problem with using a pain scale is that it’s still subjective.
A stoic person might describe their pain as a 2 on the pain scale, while another person would describe the same pain as a 6″.(2)
My personalized pain scale and pain diary were specific to my own experience of CRPS, because each person with this condition can experience a different set of symptoms and to different levels of severity. But luckily I haven’t had to track my pain again since then; it was disturbing to have to focus on my pain throughout the day – when I normally try very hard to do just the opposite!
But this is a good example of how CPRS differs from many, or most, other types of pain conditions; the sheer diversity of symptoms and types of pain at any given moment are staggering.
This is the start of CRPS awareness month, so I’m going to try to post a few pieces about what differentiates Complex Regional Pain Syndrome from other types of chronic pain conditions. Stay tuned for more!
As always, thanks so much for reading ‘-)
References:
(1) Clinical features and pathophysiology of complex
regional pain syndrome. (Review Article.) Johan Marinus, G Lorimer Moseley,
Frank Birklein, Ralf Baron, Christian Maihöfner, Wade S Kingery, et al. The
Lancet Neurology. 2011(10):7; 637-648. 01 July 2011. doi:
10.1016/S1474-4422(11)70106-5. Accessed 15 Nov 2019. Web:
https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(11)70106-5/fulltext#secd13577181e290
(2) R. Morgan Griffin; Reviewed by Brunilda Nazario. Using
the Pain Scale: How to Talk About Pain. WebMD. 09 Mar 2011. Online. Accessed 20
Nov 2019. Web (this article may be paywalled or with subscription-only access):
https://www.webmd.com/pain-management/features/pain-scale