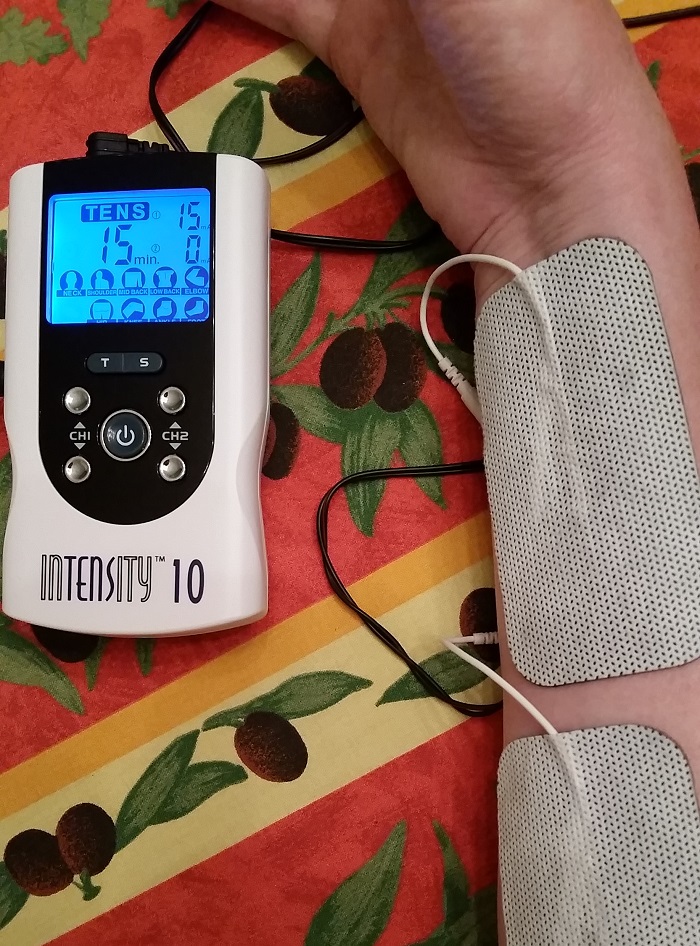
Back in June I ordered a Transcutaneous Electrical Nerve Stimulation (TENS) therapeutic device, to see whether it would help reduce – even temporarily – the severe pain of CRPS. Complex Regional Pain Syndrome is still often referred by its old name, Reflex Sympathetic Dystrophy. If you see the acronym RSD, it’s now called CRPS ‘-)
As usual, I’d done some research before agreeing to try an at-home TENS unit. There seemed to be some positive research findings about it, specifically for neuropathic pain; one type of pain that occurs in CRPS/RSD. You can read my post from June, for more information.
I found one really helpful medical journal article(1) about TENS, which aimed to:
- Provide a critical review of the latest basic science and clinical evidence for TENS
- Summarize mechanisms of action, factors that influence TENS efficacy
- Describe and critique the use of TENS for pain control in a variety of patient populations
- Present findings of systematic reviews of TENS for pain management in the last 7 years
- Highlight advances from Randomized Controlled Trials (RCT) published in the last 5–7 years, which are not included in the systematic reviews
- Offer a concise review of the basic science mechanisms for TENS
- Provide an up-to-date critique of current clinical research for TENS
This article included only 1 reference to CRPS/RSD:
TENS may offer relief to people with neuropathic pain and complex regional pain syndrome”(1).
That one sentence was enough to get me interested in trying a portable – or home use – TENS unit! It’s so rare to see this rare disease referred to in medical journal articles on pain, that a single reference to it piqued my interest!
A Canadian report noted that a “hospital survey indicates that TENS is administered predominantly by physiotherapists and actual utilization rates vary greatly from hospital to hospital as well as by application. The most frequent use, however, is for managing chronic pain”(2).
So it seems to be an accepted treatment for chronic pain, and CPRS is considered to be a chronic pain neuro-inflammatory disease. Another article, on the physician-oriented website Medscape, noted that TENS could be useful for:
Neurogenic pain (eg, deafferentation pain, phantom pain), sympathetically mediated pain, postherpetic neuralgia, trigeminal neuralgia, atypical facial pain, brachial plexus avulsion, pain after spinal cord injury (SCI)”.(3)
CPRS/RSD is considered to be sympathetically mediated pain, so this was another sign that TENS could be helpful for this disease.
So… Did it help? It’s really difficult to say whether it made any difference, because at the same time I got this $50 TENS device, I was also having day-surgery procedures at my local hospital.
I’ve had 8 different medical procedures, specifically for pain, in the day-surgery operating room (OR), since May 27th. The first six of these were stellate ganglion (nerve) blocks. The last two were Bier or IV (nerve) blocks, combined with physiotherapy, to try to break the adhesions between each joint in every finger – as well as in the wrist joint.
My neuro-anaesthesiologist suggested that I stop using the TENS machine because of these treatments, so I’ll try it again in the fall…

References:
(1) Vance, Carol GT et al. Using TENS for Pain Control: The State of the Evidence. Pain management 4.3 (2014): 197–209. PMC. Web. 28 Dec. 2017. Web:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4186747/
(2) Reeve J & Corabian P. Transcutaneous Electrical Nerve Stimulation (Tens)and Pain Management. Ottawa: Canadian Coordinating Office for Health Technology Assessment (CCOHTA). Health Technology Assessment. 01 Apr 1995. Web:
https://www.cadth.ca/transcutaneous-electrical-nerve-stimulation-tens-and-pain-management-0
(3) Kaye, Vladimir, MD. Transcutaneous Electrical Nerve Stimulation. Medscape. 09 Dec 2015. Web:
https://emedicine.medscape.com/article/325107-overview
