A few months ago a part of my world collapsed, although I didn’t realize it at the time. I was diagnosed with mild cognitive impairment, or MCI, as a result of a rare autoimmune and neuro-inflammatory disease.
I’ve had the disease since mid-2016, so had thought that I was finally starting to make my peace with Complex Regional Pain Syndrome: “a complex medical problem and, for the patient, a significant source of suffering, disability, and poor quality of life for those afflicted”.(1)
CRPS “is a chronic pain syndrome of unclear etiology”(1), meaning that physicians and researchers still don’t know what causes it. Because the cause of the disease is unknown, it has been impossible – so far! – for researchers to find effective treatments. That leaves us with:
no clear and uniform current guidelines on the treatment and management of the disease.”(1)
There are several reasons for which the name CRPS includes the word complex, and one of them is that the disease may present differently in each patient. Put another way, each patient may have a different experience of the disease; different symptoms, different progressions, different outcomes.
This can render it impossible for physicians to know which symptoms to expect in any given patient with CRPS. Despite knowing this, it was a shock when these new symptoms hit – out of the blue. MCI isn’t something that I’d ever have expected, despite the neuro-inflammatory component of the disease.
Sure enough, once I had the diagnosis I was able to find medical journal articles mentioning cognitive issues in CRPS patients. Again, there’s no treatment. With the onset of MCI, both my specialist and family physicians convinced me to take a short-term medical leave from my work. I did so – rather unwillingly – in late 2018.
That short-term leave has now morphed into long-term medical leave. With quite a lot of psychological counselling, through the hospital at which I’m treated for CRPS. The Alan Edwards Pain Management Unit (AEPMU), at the McGill University Health Centre (MUHC), takes a truly multidisciplinary approach to helping patients with chronic pain conditions.
The AEPMU team includes not only physicians, but also physiotherapists, psychologists, and other healthcare professionals to help patients like me. This time around, they’ve helped me deal with grieving for my career and for so many of the plans I had for the future.
Because the long-term leave may well signal the end of my career in biomedical ethics. The end of my dream of obtaining a doctorate, a PhD in bioethics or ethics. Bioethics wasn’t just my career, it was my passion. I would even read books on medical ethics and philosophy, on my own time, for fun!
MCI makes it almost impossible for me to read these kinds of books now, because it causes difficulties in concentrating. By the time I get to a new chapter, I can’t focus or recall what was discussed in the previous chapter(s).
It also makes it impossible for me to do my job, to evaluate requests while keeping in mind all of the relevant guidelines, laws, policies, and regulations governing a specific situation. Sometimes even writing a blog post becomes overwhelming, and I have to finish it over the course of a few days.
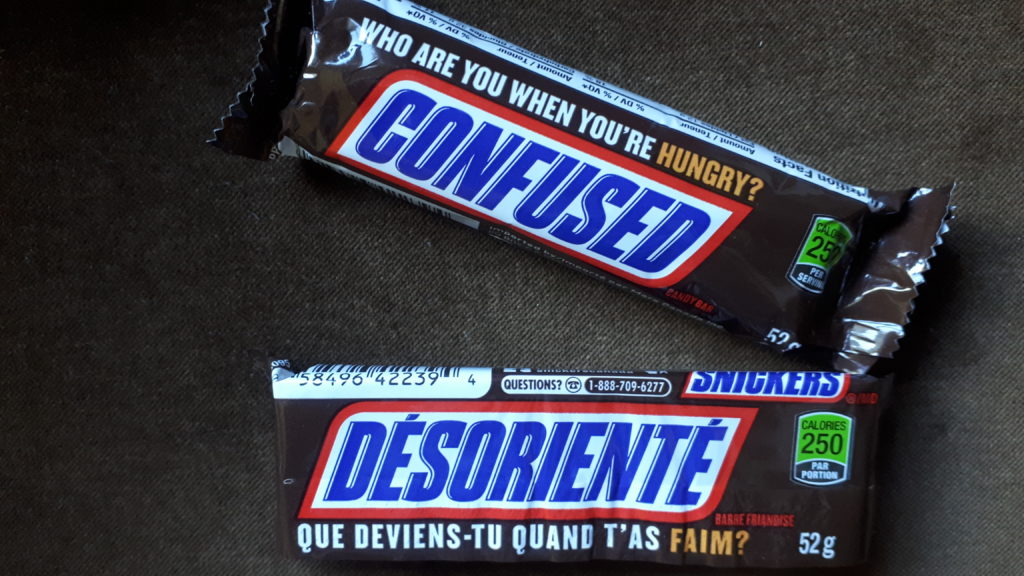
If you’ve seen any of the special wrappers for Snickers candy bars, you may have seen this one… I’ve kind of adopted it as my own these days – if only because it always makes me laugh. And yes, I do like Snickers bars 😉
How am I managing to blog these days, if I can’t work? As with much else in life, it comes down to absolutely fantastic friends and other loved ones. They won’t let me thank them here, but they know who they are!!
When I post something here these days, it will usually have been proofread by someone close to me; because I’ll sometimes write things that don’t make much sense. There might be a word missing, or one that doesn’t make sense; like the time I kept saying congratulations instead of condolences – at a funeral!
All of this is frustrating, and scary. Before the MCI appeared, I would lose myself in the pages of a book whenever I was feeling stressed or out of sorts. Ironically, now that I have the time – and arguably the most need – for the calming effects of reading, I can no longer manage it.
It’s a good thing that my family physician knows me well. Now that I’m facing a long-term medical leave, he realized that I’d need an activity to replacing reading. One of the many reasons I’ve always loved to read was to learn new things, to think.
We talked about the fact that it’s important for me to continue challenging my brain, to avoid losing any more ground to MCI:
people with MCI can take a cue from these types of findings to maintain as many healthy habits as possible.
That includes not only exercising, eating right, and staying connected with other people, but also engaging in mentally stimulating activities (particularly learning new things, like a new hobby or new language) and taking medications as prescribed.
There are no guarantees, but the evidence suggests these steps may delay or even prevent progression to dementia.”(2)
We discussed the patient advocacy and outreach that I’ve been doing since 2016, and agreed that I should continue, with some help from loved ones. My family physician understands how important this is to me, helping and reaching other patients.
But that’s not enough to stave off dementia. We had to find an activity that would challenge my brain, but in small increments. I’d need bite-sized morsels of thinking or problem-solving. I told him about an online course that I had taken online a few years ago, through an organization called FutureLearn:
online courses, programs and degrees created by leading universities, business schools and specialist organisations”.(3)
Their courses rely heavily on video clips and very short chapters or modules. Best of all, many of the courses they offer are free. These free courses are of short-duration, usually lasting 2 to 4 weeks, with about 3 hours of course activity each week. And they cover a broad range of topics.
This could be perfect, if I agreed not to take any courses that could be too challenging; my doctor doesn’t want me to become frustrated if I find myself unable to keep up with a more difficult course. So we agreed that I’d stick to general knowledge courses; learning sessions designed for the general public.
Stay tuned! I’ll post again once I’ve signed up for one of these short courses. Hopefully there will be something interesting, that begins right away ‘-)

In the meantime, I’ll be visiting the newly-renovated – and absolutely stunning – municipal library in my area. It re-opened 2 days ago, and I already adore it. It feels like a museum for books, for knowledge.
When it gets too cold and icy for cycling this winter, I may stop by this new library just to enjoy it! This new public library even has… a café! And magazines, newspapers, a games room…

©Sandra Woods 
©Sandra Woods
References:
(1) Christine Chang, Natalie Strand, Steven H. Richeimer. An
Overview of Complex Regional Pain Syndrome and its Management. Practical Pain
Management. Remedy Health Media, LLC. Online. 13 April 2016. Web:
https://www.practicalpainmanagement.com/pain/neuropathic/crps/overview-complex-regional-pain-syndrome-its-management
(2) Staving off dementia when you have mild cognitive
impairment: The shift from this condition to dementia is not necessarily
inevitable. Harvard Health Letter. Harvard University. Online. April, 2018. Web:
https://www.health.harvard.edu/staying-healthy/staving-off-dementia-when-you-have-mild-cognitive-impairment
(3) FutureLearn:
https://www.futurelearn.com

