I’m on a bit of a roll on the blog, concerning end-of-life (EoL) issues. We often think of EoL planning as important – in bioethics and medicine – mainly in terms of respect for autonomy and patients’ quality of life. An interesting study from last year added another dimension to its importance.
This study evaluated data for older hospitalized patients – those requiring major medical decisions – in intensive care units (ICUs) at 2 hospitals in the Midwestern United States(1). This study found that – 48 hours following hospitalization – almost 50% of these patients required surrogate decision-making.
The surrogate decisions(1) made for these patients – with some overlap due to certain patients for whom multiple surrogate decisions were made – included:
- Life-sustaining care, primarily code status (57%)
- Medical procedures, surgeries (49%)
- Discharge planning (47%)
The added dimension to the importance of EoL planning raised by this study is that “Patients who needed a surrogate [decision] experienced a more complex hospital course”.(1) The authors broke down some of the data for 3 very telling areas, comparing patients for whom multiple surrogate decisions were made against those who made their own decisions:
- Use of ventilator (13.2% versus 2.5%)
Artificial nutrition (14.4% versus 1.7%)
Median length of hospitalization (7 days versus 6 days)
So in addition to patients’ quality of life, and respect for their autonomy, EoL planning significantly reduced the use of both ventilators an artificial nutrition for patients making their own decisions.
Of course, it’s possible that all the patients for whom surrogate decisions were made in these 2 ICUs would have made the same decisions themselves, but I consider that to be somewhat doubtful.
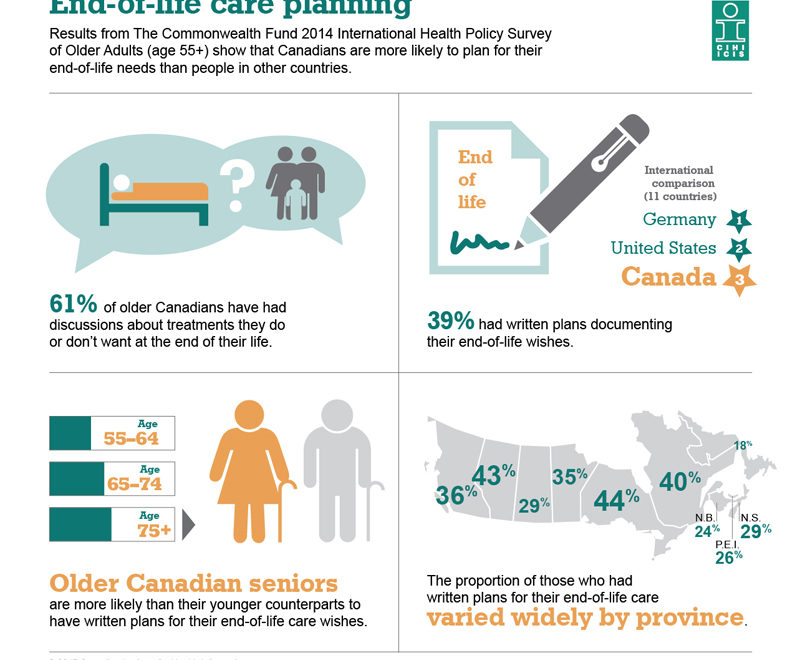
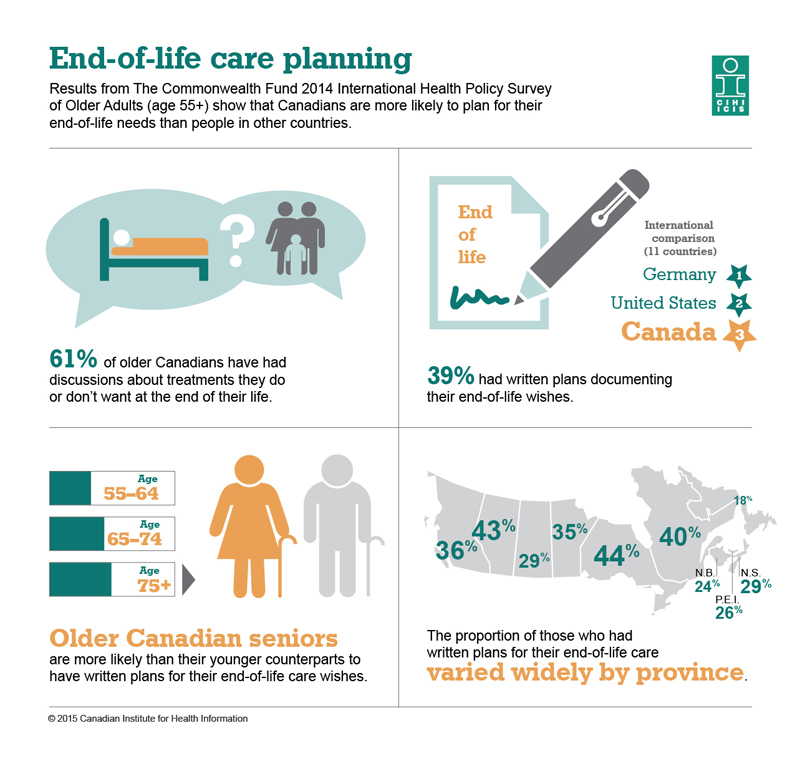
By this point, you might – rightfully – be wondering why the title of this post refers to ‘A surprise in Canada’. This surprise was included in some of the recently-released 2014 Commonwealth Fund Survey data on EoL care planning, summarized(2) by The Canadian Institute for Health Information (CIHI).
This data is specific to ‘older’ persons, those aged 55 and older, and what surprised me was that “Canadians are more likely to plan for their end-of-life needs than people in other countries”(2). I’d expected the US to top this list, but was pleasantly surprised to see Canada taking the lead on this important issue.
Canada did, however, rank below both the US and Germany for “written plans documenting their end-of-life wishes”, at 39%.(2) Perhaps unsurprisingly, the oldest Canadians were the most likely to have written EoL plans or wishes. The infographic from the Commonwealth Fund Survey (3) that I’ve included shows some of the study highlights:
The fact that EoL planning can be shown to reduce medical interventions – including the use of ventilators and artificial nutrition – might be the much-needed additional impetus for governments to take action; to raise awareness of this type of planning among their patients and caregivers.
Given the much more personal and trust-based relationships that can exist between patients and primary care physicians, tools to assist patients with EoL planning would likely be better received from a patient’s primary care physicians than from government or institutions.
One of my recent posts discussed some tools which could be provided to patients and caregivers. These tools are meant to help individuals think through their own desires and wishes for EoL, in order to then be in a position to discuss them with their loved ones.
I’d suggest that these types of tools be distributed not only to older or seriously ill individuals, but to all competent adults. We know that younger adults are much less likely to consider EoL planning, yet anyone – at any age – can fall victim to an accident or life-threatening illness.
My view has long been that we should all consider EoL planning, in much the same way that we do writing a will to deal with the care of any minors and the disposition of assets.
References:
(1) Torke AM, Sachs GA, Helft PR, Montz K, Hui SL,
Slaven JE, Callahan CM. Scope and Outcomes of Surrogate Decision Making Among
Hospitalized Older Adults. JAMA
Intern Med. 2014;174(3):370–377.
doi:10.1001/jamainternmed.2013.13315
http://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1813222?resultClick=1
(2) The Canadian Institute for Health Information
(CIHI). Commonwealth Fund Survey 2014: Caregiving and planning for end-of-life
care. 29 Jan 2015. Web.
https://www.cihi.ca/en/health-system-performance/performance-reporting/international/commonwealth-survey-2014-summaries#chap2
(3) The Canadian Institute for Health Information
(CIHI). Commonwealth Fund Survey 2014: End-Of-Life Care Planning Infographic.
29 Jan 2015. Web.
https://www.cihi.ca/en/commonwealth-fund-survey-2014-end-of-life-care-planning-infographic