As promised last month, in my post about Knowledge transfer, I’ll be blogging about interesting information that I find in medical and scientific journals on CRPS. Guess what? I’ve already found some! The American College of Emergency Physicians (ACEP) recently published an article: “What Emergency Physicians Need to Know About Complex Regional Pain Syndrome”(1)
What did this article have to say? I can’t simply cut and paste the entire article into my blog, because the doctors who wrote it are the owners of the text. Just like a book, it’s copyrighted. What I can do, though, is quote some of the article – as long as I include proper attribution. That means giving credit to the authors, and providing a link to the article; you can find this at the end of the post.
Here are some of the highlights of the article. Let’s start with a brief description of CRPS. This medical condition:
entails severe and chronic pain and disability involving a part or whole of a limb…
Approximately 60 percent of cases involve the upper limbs, with 40 percent affecting a lower limb.
CRPS typically follows a minor or moderate extremity injury, such as a wrist fracture, sprain, blunt injury, stabbing, animal bite, or elective surgery…
The disorder typically starts within four to six weeks of the injury.”(1)
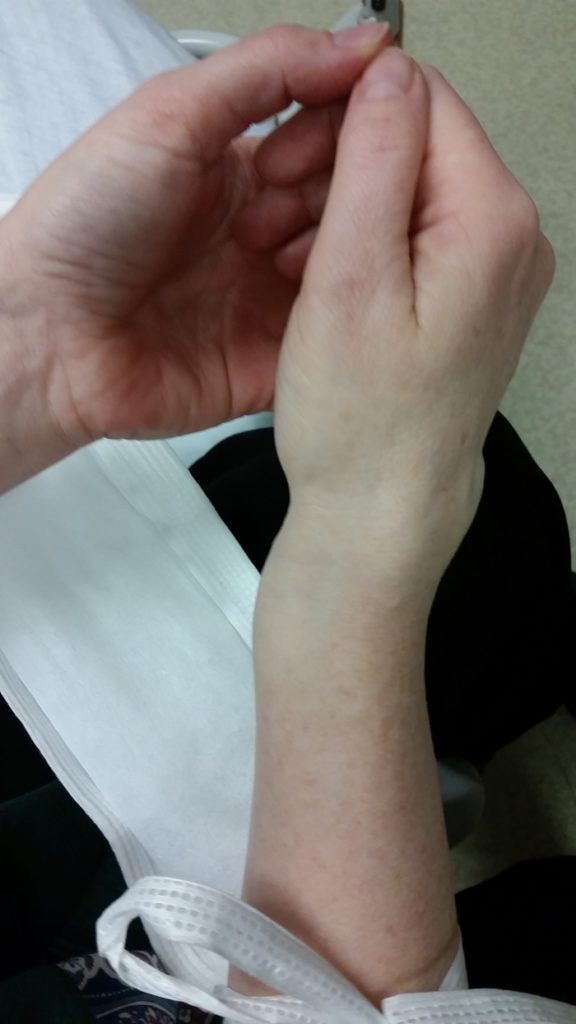
My CRPS was triggered by a Colles’ fracture, one type of broken arm. The radius bone snaps clear through, near the wrist, poking out on the top and bottom of the hand. The ends of the bone don’t always break the skin, and they didn’t in my case.

My fracture didn’t even require surgery; it healed up fine – other than the CRPS, of course! Because a Colles’ fracture triggered my CRPS, one sentence in this article really caught my eye:
“The incidence has been reported to be as high as 28 percent following Colles’ fracture, although most cases resolved after one year.”(1)
There’s a reason for hope! I was diagnosed with CRPS in May of 2016, so if this holds true then my condition could resolve – go away – by next May. Or hopefully even sooner that that… each day with this disease is a lesson in excruciating pain. Not only pain, but a host of other symptoms as well.
In fact, these doctors say that CRPS “is severely painful and treatment is difficult, involving drugs, electrical stimulation, and psychological and neurological forms of therapy.”(1).
Not only for Colles’ fractures, but for all broken bones, “splints, slings, and immobilizing devices, particularly for prolonged periods, should be avoided” when there’s a risk of CRPS. Immobilizing devices? Those would be medical items like casts and orthopaedic boots.
Despite the pain, the authors recommend that “Patients should be encouraged to use the affected extremity… Non-pharmacologic treatment options include appropriate physical and occupational therapy regimens such as isotonic strengthening, passive gentle range of motion, aerobic conditioning, aquatic therapy, and ergonomics.”
Good to hear, because I’m doing very painful – and expensive! – physiotherapy three times a week! Many CRPS patients, even here in Canada, have told me that they can’t afford any of these additional treatments. In most provinces, physical and occupational therapies are free only if they’re provided in a hospital setting. But there aren’t enough hospital therapists to go around; most of the time they work only with surgical patients.
My husband and I had set aside some money to renovate our 1991 kitchen; all beige melamine, even the counter tops! We’d planned to change the flooring in our dining room and kitchen, switch all the cabinets to wood, and add a new pantry cabinet. Instead, that money is what’s covering my physiotherapy sessions. We agreed that health was more important than a new kitchen, but I’m not sure what we’ll do when that money is gone… Another reason to hope that my CRPS goes away by next May, right?
What else was deemed important for ER doctors to know about CRPS? “Women are affected more often than men. It is most frequent in those ages 61 to 70.” Hmmm… I was under 50 when I was diagnosed with CRPS, so I suppose I’m the exception that proves the rule ‘-)
Apparently “There is evidence for posttraumatic inflammation in CRPS”, which makes sense to me. Why? Because my hand showed clear signs of inflammation, even as I was trying to convince one particular doctor that something was wrong with my hand. There were red stripes, clear signs of inflammation, running across all the finger joints on my hand.

Let’s wrap up with CRPS prevention. I read a while back, in research news, that high-dose Vitamin C supplements, for patients with Colles’ fractures, might reduce the risk of CRPS. It would be fantastic if this horrid condition could be prevented, in the future! Unfortunately, the research results don’t seem to support that approach:
“Vitamin C is proposed to prevent CRPS.
However, there is not enough evidence to recommend this for routine therapy
following, for example, a Colles’ fracture.”(1)
At this point, the only way to prevent CRPS from setting in – for at-risk patients – seems to be avoiding the use of immobilizing tools such as casts and orthopaedic boots. Precisely the types of tools which are regularly used to treat fractures and surgical patients…
Even though none of this information is breaking news, I hope you found it helpful.
As always, thanks for reading! Feel free to reach out with any comments or suggestions for the blog, or to contact me over on Twitter at @SandraWoodsMtl. Have a good day, and keep warm – it’s awfully cold out there, and CRPS despises cold weather!
Reference:
(1) What Emergency Physicians Need to Know About Complex Regional Pain Syndrome. Jonathan Glauser and Sarah Money. American College of Emergency Physicians (ACEP). 14 Dec 2016. Online. Accessed 15 Feb 2017:
https://www.acepnow.com/article/emergency-physicians-need-know-complex-regional-pain-syndrome/

