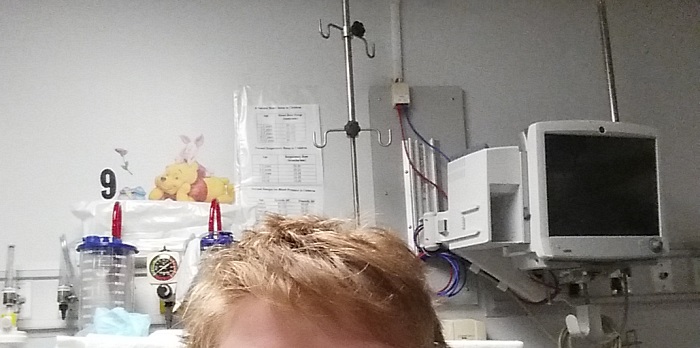
I was back at the hospital again today, for a rare neuro-inflammatory and autoimmune disease. For the second time this week. And, perhaps oddly, I felt that I was very lucky to be there – so often.
Because it means that my medical teams haven’t given up on me, or on the disease with which I’ve been struggling for almost three years now. It’s called CRPS:
Complex regional pain syndrome is a rare, chronic, and sometimes progressive condition”(1).
The medical team which has been treating me the longest consists of my family doctor and my physiotherapist (who was a physician, in another country). I see both of these healthcare professionals at the same small clinic, where they can easily share treatment information with each other – and with me.
Although only my family physician can access (or view) my medical record there, he can leave notes for my physical therapist. And my physiotherapist can write notes – or questions – about my case, to my doctor.
They are both extremely supportive, and genuinely kind people. I can feel that they each want to help me, want what’s best for my health. And they’ve continued to try, in their different ways, to find ways to make it easier for me deal with CRPS.
Also to help me deal with the impact of this chronic pain condition on my life, with a variety of symptoms that:
“include severe and continuous pain, often in part or all of a limb. It has been described as “burning” or a combination of burning and electrical shocks”(1).
For example they’ll each remind me, in their own distinct ways, that I might be trying to push my limits too far – or too quickly – for this disease. While still cheering on my efforts to not let CRPS ‘take over’ my life.
They find ways to encourage me to push the limits of CRPS, but not to a point that makes this disease worse. Which often feels like trying to balance on a high wire, with no net!

My other medical team is part of a large university health care centre; a network of hospitals and research groups. Because CRPS is classified as a chronic pain disease, I’m a patient at their multi-disciplinary pain management unit (PMU). It’s called the Alan Edwards Pain Management Unit, or the AEPMU for short.
The AEPMU covers the entire health centre network, and also receives referrals from across the province. It’s located in a large teaching hospital, and includes specialists from many areas of healthcare:
- Anaesthesiology
- Dentistry
- Family medicine
- Gynecology
- Nursing
- Palliative care
- Physiatry
- Psychiatry
- Psychology
- Rheumatology
- Social work
- And others
I’ve only been a patient there since 2016, but the AEPMU was one of the first pain centres in Canada. It’s part of a hospital that will celebrate its 200th year in 2021! This pain management unit:
tries to cure or at least improve the condition of patients living with chronic pain.
Its multidisciplinary teams follow patients closely and conduct research to better understand how pain works and the impact it has on patients, in addition to exploring potential new treatments”.(2)
I’ve been treated by several different specialists there, in anaesthesiology, interventional pain medicine, psychology, physiatry, physiotherapy… They’ve all been caring and compassionate towards me, and have shown a real desire to help.
That only begins to describe my principal doctor there. From my professional perspective, in biomedical ethics (bioethics), I know that he’s very well-known in the field of pain medicine. He’s also an important chronic pain researcher.
From my (relatively recent) patient perspective, he’s another genuinely kind person. You may have noticed that I used the word “kind” again here. If you follow this blog, you’ll know that the highest praise I can give a person is to call them “kind”. In any area or field, and in healthcare above all.
Both of these doctors, and my physiotherapist, are ‘healers’ in the medical sense of ‘healing’:
associated with themes of wholeness, narrative, and spirituality.
Healing is an intensely personal, subjective experience involving a reconciliation of the meaning an individual ascribes to distressing events with his or her perception of wholeness as a person”(3).
The kindness of each of these health professionals has been more important to me than usual, because I’ve been going through a difficult time these past few weeks; drifting.
Last month, my family doctor told me that I have “a strong will”. That I’ve proved, over and over again, that I’m strong; to him, and to others treating me for this disease. He told that I’ve also proved it to my better half, my husband; our family physician cares for both of us.
Today, the Director of the PMU told me that I’m “a fighter”. He talked with me about my positive outlook, my desire to help others.
I don’t know how to reply to these types of comments, from my physicians – the way I see it, I’m just being me. I don’t know any other way to live, can’t imagine not wanting to help others. And I can’t think of any other way to deal with this disease; its symptoms, and its setbacks.
Although I know their words are meant to be positive, I don’t know how to react to that… So I shrug them off. Change the subject. Ask a question, about something else.
It might seem to these physician-healers that I don’t appreciate their kind words, their more personal opinions. That I don’t care that they’ve taken the time to see past the patient, to see me. As a person.
But I do truly appreciate these comments, their kindness. I hope they know that. I trust that, as physicians, they understand how much of an impact their words do have. On me not only as a patient, but as a person.
That having them in my corner, to use the “fighter” analogy, will give me hope and reassurance when I most need it. That I’ll be able to look back on their comments, and draw strength from them – like drawing water from a well.
My heartfelt thanks to each of you. To everyone else, I wish you a very happy – and healthy – New Year!

References:
(1) Christian Nordqvist. Rev by Deborah Weatherspoon, PhD, RN, CRNA. “What is complex regional pain syndrome?” Medical News Today. Healthline Media UK Ltd. Updated 08 Feb 2018. On-line. Accessed 24 Jan 2019. Web:
https://www.medicalnewstoday.com/articles/184338.php#complications
(2) The Montreal General Hospital Foundation. “Vital Support for Vital Care. Annual Report 2017-2018.” 31 Mar 2018. Accessed 24 Jan 2019. Web: https://www.mghfoundation.com/en/about-foundation-codelife/annual-reports/
3) Thomas R. Egnew. “The Meaning Of Healing: Transcending Suffering”. Ann Fam Med. May 2005; 3(3): 255-262. On-line: doi: 10.1370/afm.313. Accessed 24 Jan 2019. Web: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1466870/