Last month I had my first-ever infusion, as a treatment for my rare disease; Complex Regional Pain Syndrome (CRPS). The full-body infusion of an anesthetic medication was done within the pain management unit of a university hospital, so it was very well-controlled; this isn’t something you should have done in a doctor’s office, I don’t think!
The infusion was meant to target only one aspect of my CRPS, the severe neuropathic and other types of pain that this autoimmune and neuro-inflammatory disease causes. You can read more about the infusion itself in this post from last month.
Today I’d like to focus on pain scales, the rating systems used by chronic pain clinics that ask a patient to select the level of their pain from a list or visual images. Some pain scales use a kind of happy face type of pain rating, with a happy face meant to indicate no pain and a screaming face to show the most severe pain.
From both my bioethics and patient perspectives, these pain scales leave a lot to be desired. First off, as I explained last year, I experience my CRPS pain as layers of pain. Imagine a layer cake, with seven layers, each one a slightly different thickness. At any given moment, I’ll usually be feeling seven specific and distinct types of pain, to varying degrees of severity. Like a lumpy layer cake of pain!
But the pain scale that I had to use, to track my pain levels after my infusion last month, only has room for one type of pain; by that I mean that the form assumes that a patient is only experiencing one type of pain. That’s never the case for me, not with CRPS. In part because there are both autoimmune and neuro-inflammatory symptoms.
The former causes different types of joint pain, while the latter is responsible for my neuropathic pain; including a particularly obnoxious skin sensitivity called allodynia.
One definition of allodynia is “pain due to a stimulus that does not usually provoke pain”(1), which isn’t all that helpful unless you already know what it feels like! In my case, as for most patients with CRPS, allodynia is an extreme sensitivity of the skin in the affected area – my right hand and arm – to the lightest touch, temperature change, or even air current.
A gentle breeze can trigger this pain, even my own breathing; for example if my hand is in my lap! I can’t bear to have most clothing touch my hand or lower arm, so I’ve had to revamp my wardrobe. I despise shopping at the best of times, but it was so much worse because I can’t let any of the fabric touch my hand while I’m trying things on! Now all my sweaters and suit jackets have a three-quarter length sleeve, and I can only wear coats and parkas that have a super-soft fleece or satiny lining.
Whoops, I’ve wandered off topic again! Let’s get back to the topic of pain scales… One of the problems, as we’ve seen, with the pain scale I was given after my infusion is that it was meant to capture only one type of pain at a time. Another issue I had with this pain diary is that I don’t know how exactly to rate my pain; which number to pick on that one to ten scale.
I don’t think I rate pain the same way now that I did before living with CRPS for over two years. The description for ten out of ten on the pain scale is usually ‘the worst pain imaginable’. But my daily pain from CRPS goes past what I could have considered the worst pain imaginable, before I developed this condition. So how do I account for that? Some pain specialists have noted the same issue:
Of course, one inherent problem with using a pain scale is that it’s still subjective.
A stoic person might describe their pain as a 2 on the pain scale, while another person would describe the same pain as a 6.″(2)
This all leaves me with something of a dilemma. To complete a standard pain scale at my pain management unit, I’ve always tried to very roughly average out the different levels of pain that I’ve experienced within the specified timeframe, so I’d report 6+6+7+8+8 as “7”. Or 5+5+9+9 as “7”. But this doesn’t give a true report of my pain situation.
This averaging effectively, if unintentionally, cancels out the higher and lower ends of the spectrum of pain severity. Added to that, I also try to very roughly average out the different types of pain sensation that I experience (e.g. allodynia, joint pain, burning or freezing neuropathic pain, swelling).
These two issues leaves me feeling that the standard pain scale and diary are much less relevant to CRPS than to other pain conditions. From a bioethics perspective, I wonder about accuracy of patient reports in these situations – for both clinical care and research purposes.
From a patient perspective, it’s frustrating to try to fit CRPS symptoms into data collection tools which don’t account for the multiple types of pain of this disease. Other patients have told me that CRPS often is their “worst pain imaginable”, but that they hesitate to rate it as a “10” for fear they’ll be labelled as complaining, exaggerating, or seeking medication.
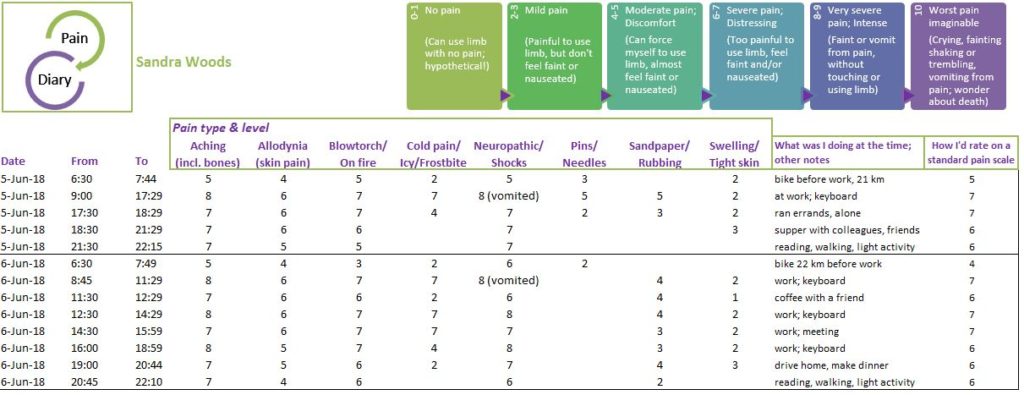
So, after my infusion, I decided to try to create my own version of a pain diary; specifically tailored to my own CRPS symptoms. This one accounts for the multiple pain sensations I experience; my layer-cake of pain. Before I could create my own pain diary, I first had to revise the descriptions in the commonly-used pain scale – to avoid inconsistencies in my pain reporting.
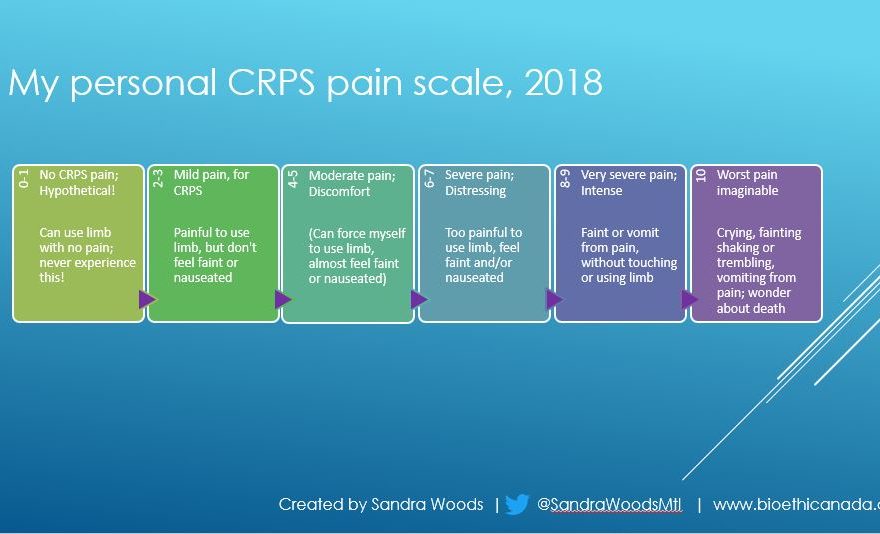
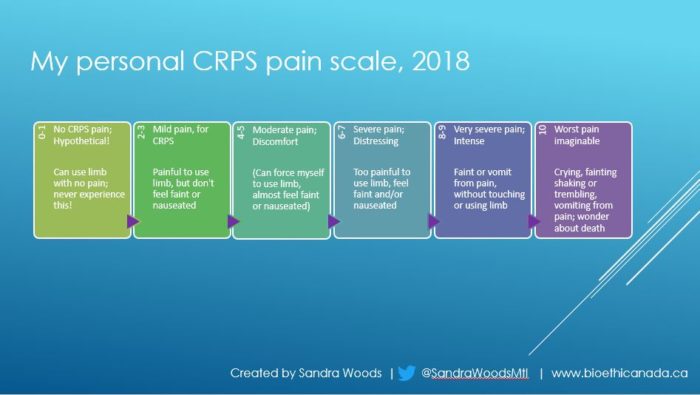
For simplicity’s sake, I kept the standard phrasing (e.g. “worst pain imaginable”). In the original version of my individualized pain diary I had reported separately on each of my finger joints and my wrist. That quickly became a tracking nightmare, so I gave up on that aspect of my diary fairly quickly! This is what I came up with, my altered descriptions for the one-to-ten pain ratings:
I also realized – in the course of this experiment in creating my own pain scale and diary – that I really don’t like keeping a pain diary. Keeping track of my pain throughout the day was disturbing from a psychological perspective; I try not to focus on my pain, but keeping a diary forced me to do just that.
Filling in my pain diary brought me as close as I have ever been to feeling depressed or anxious – ever. This entire experience leaves me wondering about the impact of pain diaries on patients who are already suffering with anxiety or depression, and whether anyone is researching the psychological impact of these diaries.
One of these days I’d like to raise this issue with my own pain specialist, but there are always so many patients waiting to see him that I hate to take any of his time for something that’s not directly related to my treatment plan.
Whether you’re a chronic pain patient, or a researcher or specialist, I hope you found this post interesting. If you want to use any of my ideas, I’d ask that you credit me; even better, reach out via Twitter or Instagram to ask about collaborating on a research or treatment project to develop better pain reporting tools for CRPS.
As always, thanks so much for stopping by the blog ‘-) Have a lovely day, filled with moments of the beauty of springtime!
References:
(1) Troels S Jensen, and Nanna B Finnerup. Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms. The Lancet Neurology. Review article. 2014(13);9;924-935. Sep 2014. Online doi.org/10.1016/S1474-4422(14)70102-4. Web:
https://www.thelancet.com/journals/laneur/article/PIIS1474-4422(14)70102-4/fulltext
(2) R. Morgan Griffin; Reviewed by Brunilda Nazario. Using the Pain Scale: How to Talk About Pain. WebMD. 09 Mar 2011. Online. Accessed 20 Nov 2019. Web (may be paywalled or with subscription-only access):
https://www.webmd.com/pain-management/features/pain-scale