Something I’ve noticed, across a few hospitals and specialized clinics, is that the tools used to rate pain often aren’t adequate. Not for my specific disease, at any rate.
Let’s start with a quick rundown of some of the signs and symptoms of Complex Regional Pain Syndrome (CPRS). These are generally limited to the area of the body affected by the disease:
- Allodynia; a painful skin sensitivity to cold, fabrics (clothing), a touch, a breeze, etc.
- Difficulty sleeping, due to pain and other symptoms
- Joint pain due to the formation of ankyloses, similar to scar tissue, inside affected joints
- Joint rigidity or stiffness, which can contribute to ‘claw hand’
- Limitations of movement, range of motion
- Neuropathic pain, often severe, which can include sensations of extreme cold or heat; burning or freezing pain
- Oedema (swelling), and related pain
- What physicians call vasomotor, sudomotor, and trophic dysfunction; these usually show up as different patterns of sweating, hair growth, nail growth, and skin temperature as well as discolouration of the skin and other issues
- Other unexplained symptoms, for example the painful feeling that the skin of the affected area is constantly being rubbed with sandpaper or being stung by insects
Pain is noted several times in this list, because CRPS often – as in my case – involves many distinct sensations of pain. Unfortunately people with CRPS may experience all of these concurrently, and at varying levels of severity.
Each time I visit my multi-disciplinary pain management unit, there are pre-printed written questions about my perceived pain. This is necessary, of course, to provide appropriate treatment as well as to track a patient’s progress over time. Or lack of progress, as the case may be.
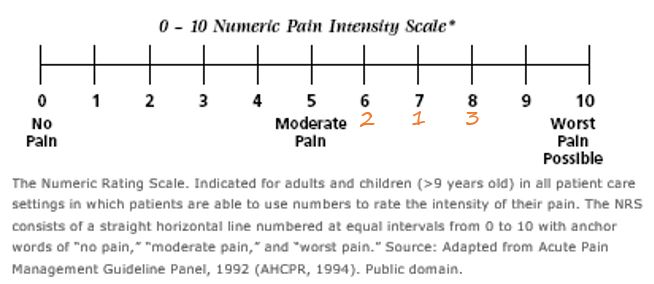
This data is generally collected by means of a form or questionnaire, which asks that I circle the level of pain for each pre-determined question or statement. Or using a pain rating scale; a line with numbers along its length – of 0 (no pain) to a higher number (worst pain imaginable).
The higher number used at my hospital is 10. Other patients I’ve touched base with have seen pain scales going up to 5, or even 20.
There are a variety of these scientifically validated pain scales, in use at different hospitals and clinics around the world. I’ve often joked that it’s the same concept as many customer surveys, those that you might receive by email after having made an online purchase.
For pain scales, the questions might include:
- How is your pain today (circle the level from 0 to 10)?
- Rate your pain level over the past week, from 0 to 10
- For the past month, what was your overall pain level (from 0 to 10)?
- Over the last week, what was the lowest level of pain that you felt, from 0 to 10?
The problem I’ve encountered with these pain rating scales is that I almost never experience the same level of pain – at any given time – for each of the different types of pain that I deal with on a daily basis. The joint pain may be a 6, while the neuropathic pain is a 9. Or I might have extreme pain from swelling one day, when it’s been more bearable for the past few days.
One of the trickiest things about CRPS is that the symptoms aren’t static – they fluctuate. No day is the same, not for me at any rate. And these pain levels change over the course of each day. This makes it exceedingly difficult for me to rate my pain for a specific day, week, or month, using one single pain questionnaire.
It’s possible that a pain scale has already been designed, and validated, to address this particular issue. If it did already exist, however, I’d have expected to have seen it by now – given that I’m treated at a university-hospital pain management unit. So I have to assume that there is no pain rating scale yet, to address multiple distinct pain sensations all experienced at the same time.
My solution to this dilemma has been to try to average out the various types of pain, and to rate the average. But that skews the high pain ratings downwards and skews the low pain upwards; it makes my high levels of pain seem lower, and vice-versa. This no doubt provides data that is clinically questionable, or perhaps even unreliable, to my pain management team.
I’ve realized that this disease is one that I’d have called ‘messy’ – back when I was working in clinical (medical) research ethics – because it doesn’t follow a regular pattern. One day the symptoms can be almost bearable, while the following day they’re absolutely horrific.
CRPS can resolve, simply disappear, in some people. For other patients the condition never loosens its grip, instead progressively worsening. I’ve heard of cases in which an individual seemed to be improving, only to later get worse. It’s an unpredictable disease in many ways. And no one really understands why it starts, or how best to treat CRPS. There’s no cure.

Based on that insight, I like to think that it would probably be more sensible to have CRPS patients rate their pain as the messy beast that it is. To come to terms with that, I’ve tried to describe my pain in terms of ‘layers’. I can differentiate between the types of pain I’m feeling; separate any one from the others, and rate it independently. Just as you can see the layers on a cake, once you cut into it, I can feel the different layers of my CRPS pain.
It would be very easy for me to provide a different rating number for each of these types of pain. This really wouldn’t be as complicated as it sounds! If someone were to ask for patient suggestions, for a better way to rate CRPS pain, I’d have two ideas.
First off, instead of a line-based scale to rate pain it could be a list format. A patient could have all of their specific CRPS pain types listed on a pre-printed form, and rate each one for any specific point in time. This could still be done using the traditional 0 (no pain) to 10 (worst pain imaginable) scale.
As an example, these are the specific and distinct types of pain that I’m experiencing at this very moment:
- Allodynia
- Burning pain
- Cold pain
- Joint pain, fingers
- Joint paint, wrist
- Neuropathic pain, like electric shocks
- Oedema/swelling pain
Second, if the pain centre or clinic preferred to use a pain scale showing the line or bar scale, each CRPS patient could have their own list of pain sensations. These could be numbered using roman numerals (i, ii, iii, iv…) or letters (a, b, c, d…).
Instead of circling the number for only one pain level, on a line showing 0 to 10, a patient could write in the numbers for each of their distinct types of pain under the appropriate pain level. The scale would then show the pain level for each of the particular pain sensations experienced by that individual.
I’ve created a sample version, for a CRPS patient who experiences only three distinct types of pain; 1) allodynia, 2) burning pain, and 3) pain from oedema or swelling:
Either option would provide much more accurate – truer – data on the pain levels experienced by CRPS patients. It would definitely be more accurate than the current method, in which patients like me try to rate all their different pain levels – combined – as a single dot along the line of a pain scale.
Hopefully someday someone will ask a CRPS patient for their perspective on better ways to rate the pain they experience as a result of this nasty disease. In the meantime, I’ll have to continue averaging out my many types of pain to arrive at an inaccurate and non-representative number for any given time period; as requested by the current pain scales.
Or, if such a pain rating system already exists, perhaps it will be adopted by a larger proportion of pain management centres.
As always, thanks for reading!

