To start the New Year yesterday, I thought back to all the good things that took place in 2016. This has been a habit of mine throughout all of my adult life. On New Year’s Day, rather than being sad that the winter holiday period is coming to an end, I focus on thankfulness.
My friends would say that I do this all the time, being an eternal optimist, but on January 1st of each year it’s a much more involved process for me. I take out the photo album to look at all the images from the past year, although these days it’s more a case of scrolling through the photos on my phone! Which reminds, I really should download this year’s photos for safekeeping…

Each time we attend an event, I set aside the concert tickets, museum stubs, special event passes, and invitations to celebrations such as baby showers, weddings, and even memorials. I sort through these, on the first day of the New Year, taking the time to recall each event. If I have time that day, I’ll create a few scrapbooking pages; a quick visual summary of our year.
For 2016, as with every year since our lives entwined, I was most thankful for my husband. My best friend and soul-mate, he’s the person who has always encouraged me to follow my dreams – to follow my heart. Then thankfulness comes almost in waves, each wave for a different loved one; whether family or friend. Then for all what I’ve done throughout the year, places I’ve been, people I’ve met, things I’ve learned.
Looking back on this past year – focusing on the positive aspects – one thing stood out from all the rest, as being completely different. Are you wondering what that could that have been? It was finding a place within healthcare in which I felt believed, listened to, and heard. Why?
In early March of 2016, I fractured my right arm. A simple slip on a patch of black ice, a cleanly snapped bone. Nothing complicated, but an obvious fracture. I even drove myself home, so I could change into comfy clothes before my husband brought me to the hospital. My military friends will all be rolling their eyes at this point, thinking: “Yeah, that’s straight-up Sandy.” Although probably with a few more colourful words thrown in ‘-)

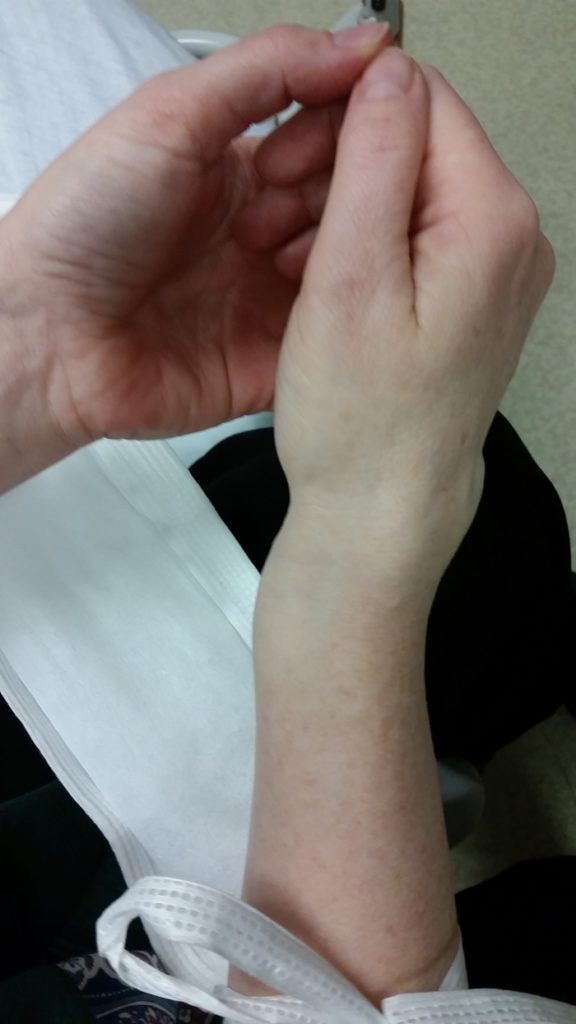
The fracture healed properly, without any need for surgery. Within about a week of that injury, though, I knew that something wasn’t right. I was experiencing more pain after the fracture than I had at the time of the injury. The fingers on the injured arm were more swollen than they had been immediately after the fracture. My field in bioethics, or biomedical ethics, and I’ve spent a long time working in healthcare. I’ve also taken, and then taught, military First Aid training courses.
It simply didn’t make sense to me that I’d have more finger pain and swelling post-fracture. And that pain was excruciating, a burning pain. I‘d describe as feeling that someone was holding a blowtorch to my fingertips. As the weeks went by, that burning sensation spread upward towards my wrist.
When I raised this issue with the physician at my local community hospital, who had been assigned to my post-fracture follow-up care, he dismissed me. Repeatedly. It took until the end of May for him to finally agree to get a second opinion; he brought in another physician, who didn’t even need to examine me. He leaned on the door frame of the examining room, asked me a couple of questions, and provided a 3-letter diagnosis. RSD. He kindly wished me “Good luck” before heading back out the door.
RSD is Reflex Sympathetic Dystrophy, now called CRPS for Complex Regional Pain Syndrome. Are you wondering why I’m writing about this, in a post about positive events in 2016? I’m getting there, I promise!
During the almost three months in which I knew that something was wrong with my right hand, I was dismissed. Told – by physicians, nurses, and other healthcare professionals – that I was over-reacting. One, in a hospital, even told me to “stop exaggerating” about the pain I was experiencing. At work, colleagues would tell me things like: “My 12-year old son broke his arm a few weeks ago too, and he’s not complaining about it!”
There I was, a bioethics professional, someone who’d worked in hospital; unable to find a way to make myself heard as a patient. It was such a frustrating experience, being in such severe pain yet unable to convince any of the professionals involved in my medical care.
In August my local community hospital ended my follow-up care for CRPS, saying that they had “done all they could for me”. It took some insistence on my part, but they finally referred me to a chronic pain clinic at a university hospital in our city centre area. After months with CRPS, I qualified as a chronic pain patient.
And this, ladies and gentlemen, is the point at which I get to talk about that one positive occurrence in 2016 that stood out from all the others. As being different from concerts, travel, weddings, and other special events with family and friends.
I was invited to attend a ‘potential patient orientation session’, on October 25th, at that chronic pain clinic. The Alan Edwards Pain Management Unit (AEPMU) is part of the McGill University Health Centre (MUHC), and is located within one the MUHC’s hospitals; the Montreal General Hospital (MGH).(1)
This orientation session was a presentation, with PowerPoint slides, to a group of people who had been recently referred to the AEPMU because they were living with chronic pain. I’d expected to see an administrative employee giving this presentation. Instead, it was the Director of the AEPMU who took the time to speak with us – as potential patients.
Finally, it felt as though there was hope. The approach of the AEPMU, he said, was to treat chronic pain as a disease in and of itself. That even though – in some cases – it wouldn’t be possible to eliminate or even significantly reduce a person’s pain, the AEPMU might be able to help them to live better with their pain. You can read an online “Message from the director” of the AEPMU at: https://www.mcgill.ca/paincentre/about-us/message-director.
During the presentation it was explained that the AEPMU is a multidisciplinary pain management clinic, with specialist physicians from different areas of medicine working alongside nurses, physiotherapists, psychologists, and other healthcare professionals.
All with the same goal, to make the lives of people living with chronic pain better. If, of course, they weren’t able to eliminate that pain! Unfortunately, there can be a wait to be evaluated by the AEPMU, because the number of patients referred far exceeds the clinic’s capacity to treat them.
Despite the possibility of a(nother) wait, the AEPMU could offer hope. Somewhere patients wouldn’t be told to “stop exaggerating”, or made to feel demeaned or diminished because they’re unable to “just deal with” their pain.
You might be thinking that this was only an initial presentation, an orientation session. That it’s easy to say the right things, to seem concerned about the well-being of patients, while one’s actions don’t reflect that. The AEPMU team, though, has lived up to that promise so far. I was accepted as a patient there fairly quickly; apparently CRPS is prioritized in the pain clinic’s triage process. Likely because:
CRPS patients’ risk for suicide has been reported to be considerably higher than that not only of general populations but also of other chronic pain populations.”(2)
I now suspect it was also for that reason that the AEPMU Director asked to speak with me for a moment after the presentation. To be honest, I expected to be told that I wouldn’t even be considered for acceptance as a patient. CRPS is an invisible illness, and I seem fine. I’m still working, thrilled to have started my dream job earlier this year, combining bioethics and philanthropy. Although some days I do wonder how I made it through the day, despite excruciating pain.
I still ride my bike, go hiking, socialize with friends. I’m not bedridden by pain, and had so often been made to feel – by other healthcare professionals – that I should be able to somehow get past the pain of CRPS. When the APEMU Director pulled over a chair, and sat across from me at the back of the conference room in which he had just presented the orientation session, I wasn’t expecting good news.
A surprise was in store. What he said to me was:
We know what CRPS is. We know what you have, what you’re going through, and we’re going to help you. Just hold on. You’ll be the first patient we see in this group. Just hold on a bit longer.”
I didn’t realize that tears were streaming down my face, until he handed me a tissue. What I do recall, very clearly, is such an overwhelming feeling of relief. That I didn’t have to try to explain what I was experiencing, that I wasn’t going to again be told to “stop exaggerating” at another hospital.
It immediately felt as though I’d found a safe place – to be a patient, a person. That the impact of this disease, of CRPS, wasn’t something that I’d have to struggle to communicate to another disbelieving physician. That feeling, of the AEPMU being my ‘safe place’ remains intact.

My first appointment as an AEPMU patient, my initial evaluation, was on November 15th. It would have been sooner, but I was chairing meetings at work on all of the earlier dates that they’d proposed. And you know what? They walked the talk!
Every single person at the pain clinic with whom I had the pleasure to speak that day, from their receptionist to the physician who’ll be treating me, was kind. If you’ve been following this blog from its original bioethics days, you’ll know that I value kindness above almost all else in healthcare (e.g. my posts on kindness in healthcare, from 2012 and from 2016).
To say that a healthcare professional or employee is kind, that’s the highest praise that I can give… from any of my perspectives; bioethics, caregiver (to my mother, before she passed), patient. No surprise, really, given that it’s also the attribute I value most in my friends! ‘-)
As for treatments at the AEPMU, I left my first appointment with some new prescriptions which have already helped to take the edge off my pain levels. Plural, because CRPS causes several different types of pain, like layers on a cake. Next week I’m scheduled to have a nerve block at the AEPMU. This procedure will be a new one for me, an axillary brachial plexus block. Stay tuned for details of that, later this month.
This post is about thankfulness, about looking back on the past year in terms of the good things that happened. Finding my ‘safe place’ at the AEPMU? That was something for which I am truly thankful.
As always, thanks for reading. Feel free to leave a comment, to reach out over on Twitter or Instagram. May 2017 be a good year for you, filled with moments of joy and laughter. Happy New Year!
References:
(1) Alan Edwards Pain Management Unit: Treatment, Education, Research. McGill University. Online. Accessed 01 Jan 2016. Web:
https://www.mcgill.ca/paincentre/
(2) Executive function and suicidal risk in complex regional pain syndrome: preliminary study. Sin, M. et al. The Journal of Pain, Volume 16, Issue 4, S19. Apr 2015. Abstracts Presented at the 34th Annual Scientific Meeting of the American Pain Society, 13 May 2015 – 16 May 2015. Web:
https://www.jpain.org/article/S1526-5900(15)00125-X/fulltext

