The two-day Play the Pain(1) discussion forum, comprised of workshops and scientific presentations, took place October 1st and 2nd. There were so many different activities packed into those two days, and so much information to process, that I’m writing about each of the most interesting sessions separately.
Today I’d like to share with you my favourite among the scientific presentations at Play the Pain: “NeuroScientific Boundaries”, which discussed the use of brain imaging for research into both chronic pain and temporary pain sensations.
I’ve already written about one of the participatory workshops, on creative writing and pain, and will update you on others over the coming days. Stay tuned!
The scientific presentation that I’d like to summarize today was given by Christophe Tanguay-Sabourin. He’s a student at McGill University, specializing in “brain imaging and clinical applications of neuroinformatics for chronic non-cancer pain”(2) – or CNCP for short.
Christophe is also a member of the Quebec Network of Junior Pain Investigators (QNJPI). If you ever venture over to Twitter, you can follow him there at @TanguaySabourin.
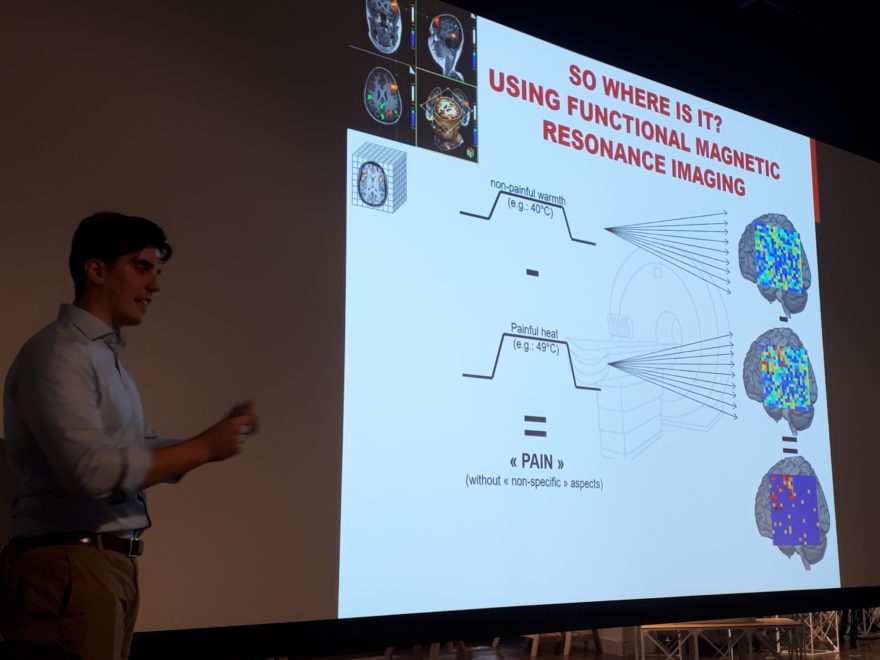
He presented results of research using functional magnetic resonance imaging (fMRI) to investigate which portions of the brain are involved in the perception of non-painful heat (e.g. 40C) and painful heat stimuli (e.g. 49C).
Although this is very interesting, I don’t view it as particularly helpful for the study of CRPS – or other chronic pain conditions – because the temporary application of a painful stimuli on a health volunteer is unlikely to provide the same fMRI results as a chronic pain trigger on a patient living with constant and severe pain.
That said, many feel that any research on pain is good research on pain! In that sense, this type of research may someday lead to new discoveries that do apply to CRPS and other neuropathic pain conditions ‘-)
What interested me most about Christophe’s presentation was his discussion of complementary and alternative medicine (CAM), because it’s unusual for researchers to include these in their discussions. Yet many chronic pain patients rely on these practices or services, often in addition to conventional medicine and therapies – such as physical or occupational therapy.
He began this part of the presentation with the following statement, with which I fully agree:
Even after considering individual differences, it remains that [a] multidisciplinary approach is currently the only effective treatment approach”.(3)
A few of the CAM included Christophe’s discussion were:
- Acupuncture
- Ayurvedic medicine
- Indigenous healing practices
- Mind-body healing
- Mindfulness meditation
- Movement-based therapies
- Nutriceuticals (e.g. anti-inflammatory foods)
- Osteopathy
- Qi Gong
- Traditional Chinese medicine
Christophe wrapped up his presentation by referring to the extensive experience of a well-known chronic pain clinician and researcher, Dr. Yoram Shir. Dr. Shir is the Director of the Alan Edwards Pain Management Unit (AEPMU) at the McGill University Health Network (MUHC).
The AEPMU is the chronic pain clinic at which I receive treatment for Complex Regional Pain Syndrome (CRPS), and I’ve had the pleasure of meeting Dr. Shir. A few months ago, I provided a patient perspective to a training session being conducted by Dr. Shir; for 2nd year medical students, at McGill University.
Specifically, Christophe mentioned three of the conclusions that Dr. Shir has drawn from his vast clinical experience treating chronic pain patients:
- “There are not enough scientific data on CNCP”
- “Multiple factors dictate [the] approach to the individual patient”
- “Team work is essential”(4)
This presentation ended with one of my favourite lines from Dr. Shir:
Chronic pain therapy is a bit of an art, a bit of voodoo medicine, and a bit of science.”(4)
After his presentation, I had a couple of questions for Christophe; for example whether the larger team within which he’s studying has found any way to use fMRI to measure the actual perceptions of pain of individuals living with chronic pain rather than applying a painful stimulus to a healthy volunteer. [They haven’t, yet.]
This led to a truly fascinating conversation about his neuroscience research, and also about some of the researchers and clinicians we’ve each met; him as a student and researcher, and me as a patient partner at various chronic pain conferences and events.
Next up on the Play the Pain agenda were a series of five-minute mini-presentations on the potential of music to provide analgesia – pain relief – for chronic pain. That will also be the topic of my next post about the Play the Pain event ‘-)
In the meantime, if you’re interested in the neuroscience of chronic pain, consider attending the upcoming TEDtalk-style PAINtalk event here in Montreal! It’s free, and open to the public, but reservations are required. I’m helping the organizers spread the word among people living with chronic pain, a kind of informal patient partner ‘-)
References
(1) Play the Pain. Media Health; Concordia University [Media Health Lab is a collaborative initiative supported by Concordia University PERFORM Centre and The Milieux for Arts, Culture and Technology]. 2019. Online. Accessed 06 Oct 2019. http://media-health.ca/events/play-the-pain-4thspace/
(2) Christophe Tanguay-Sabourin: @TanguaySabourin. Twitter profile. Undated. Online. Accessed 06 Oct 2019.
https://twitter.com/tanguaysabourin?lang=en
(3) Christophe Tanguay-Sabourin. Presentation: NeuroScientific Boundaries, at Play the Pain, 01 Oct 2019.
(4) Yoram Shir, quoted by Christophe Tanguay-Sabourin. Presentation: NeuroScientific Boundaries, at Play the Pain, 01 Oct 2019.